How Medicare SNPs work
Special Needs Plans (SNPs) are a type of Medicare Advantage plan in Florida designed to provide specialized care and services for people with specific chronic conditions, disabilities, or other health care needs. SNPs in Florida are required to provide all the same benefits as traditional Medicare Advantage plans, but they also offer additional benefits and services tailored to the specific needs of their members. Qualified Medicare recipients can join a SNP at any time.
There are three types of Special Needs Plans in Florida:
- Chronic Condition SNP (C-SNP): These plans are designed for Medicare patients in Florida with chronic conditions such as diabetes, heart disease, or cancer.
- Dual Eligible SNP (D-SNP): These plans are designed for Floridians who are eligible for both Medicare and Medicaid, and often provide additional benefits and services beyond what is covered by traditional Medicare. Medicaid is a joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid.
- Institutional SNP (I-SNP): These plans are designed for Medicare recipients who reside in institutions such as nursing homes, and provide specialized care and services that meet the unique needs of these individuals. If you live in an institution, make sure that plan providers serve people where you live. Find out more about where SNPs are offered.
SNPs in the state of Florida are required to have a network of health care providers who specialize in the care of the targeted population. Members of SNPs typically have lower out-of-pocket costs and receive additional services such as care coordination and disease management programs.
- You have Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance) .
- You live in the plan's service area
- You meet the plan's eligibility requirements for one of the 3 SNP types:
- Chronic alcohol and other dependence
- Certain autoimmune disorders
- Cancer (excluding pre-cancer conditions)
- Certain cardiovascular disorders
- Chronic heart failure
- Dementia
- Diabetes mellitus
- End-stage liver disease
- End-stage Renal Disease (Esrd) requiring dialysis (any mode of dialysis)
- Certain severe hematologic disorders
- HIV/AIDS
- Certain chronic lung disorders
- Certain chronic and disabling mental health conditions
- Certain neurologic disorders
- Stroke
2. Institutional SNP (I-SNP) - You live You live in the community but need the level of care a facility offers, or if you live (or are expected to live) for at least 90 days straight in a facility like a:
- Nursing home
- Intermediate care facility
- Skilled nursing facility
- Rehabilitation hospital
- Long-term care hospital
- Swing-bed hospital
- Psychiatric hospital
- Other facility that offers similar long-term, health care services and whose residents have similar needs and health care status as residents of the facilities listed above
3. Dual Eligible SNP (D-SNP) - You’re eligible for both Medicare and Medicaid. D-SNPs contract with your state Medicaid program to help coordinate your Medicare and Medicaid benefits.
Each Medicare SNP limits its membership to people in one of these groups, or a subset of one of these groups.
For example, a Medicare SNP may be designed to serve only people diagnosed with congestive heart failure. The plan might include access to a network of providers who specialize in treating congestive heart failure. It would also feature clinical case management programs designed to serve the special needs of people with this condition. The plan's drug formulary would be designed to cover the drugs usually used to treat congestive heart failure. People who join this plan would get benefits specially tailored to their condition, and have all their care coordinated through the Medicare SNP.
A Formulary is a list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
Insurance companies can decide that a plan will be available to everyone with Medicare in a state, or only in certain counties. Insurance companies may also offer more than one plan in an area, with different benefits and costs. Each year, insurance companies offering Medicare SNPs can decide to join or leave Medicare.
If you don't have both Medicare and Medicaid (or get other help from your state paying your Medicare premiums), your exact costs will vary depending on the plan you choose. In general, you'll pay the basic costs of having a Medicare Advantage plan.
For example, a Medicare SNP for people with diabetes might use a care coordinator to help members do these things:
- Monitor their blood sugar
- Follow their diet
- Get proper exercise
- Schedule preventive services (like eye and foot exams)
- Get the right prescriptions to prevent complications
Example:
Mr. Johnson joined a Medicare SNP that only serves members with both Medicare and Medicaid. Mr. Johnson loses his Medicaid eligibility. Medicare requires Mr. Johnson's plan to disenroll him unless he becomes eligible for Medicaid again within the plan's grace period.
The grace period is at least one month long, but plans can choose to have a longer grace period. If you lose eligibility for the plan, you'll have a Special Enrollment Period to make another choice.
This Special Enrollment Period starts when your Medicare SNP notifies you that you're no longer eligible for the plan. It continues during the plan's grace period, and if you're disenrolled from the plan at the end of the grace period, it continues for 2 months after your coverage ends. It's very important to review your coverage options at this time to make sure you continue to have the Medicare health and prescription drug coverage you want.
Can I get my health care from any doctor, other health care provider, or hospital?
Some Florida SNPs cover services out of network and some don’t. Check with the plan to see if they cover services out of network, and if so, how it affects your costs.
Medicare SNPs typically have specialists in the diseases or conditions that affect their members.
Are prescription drugs covered?
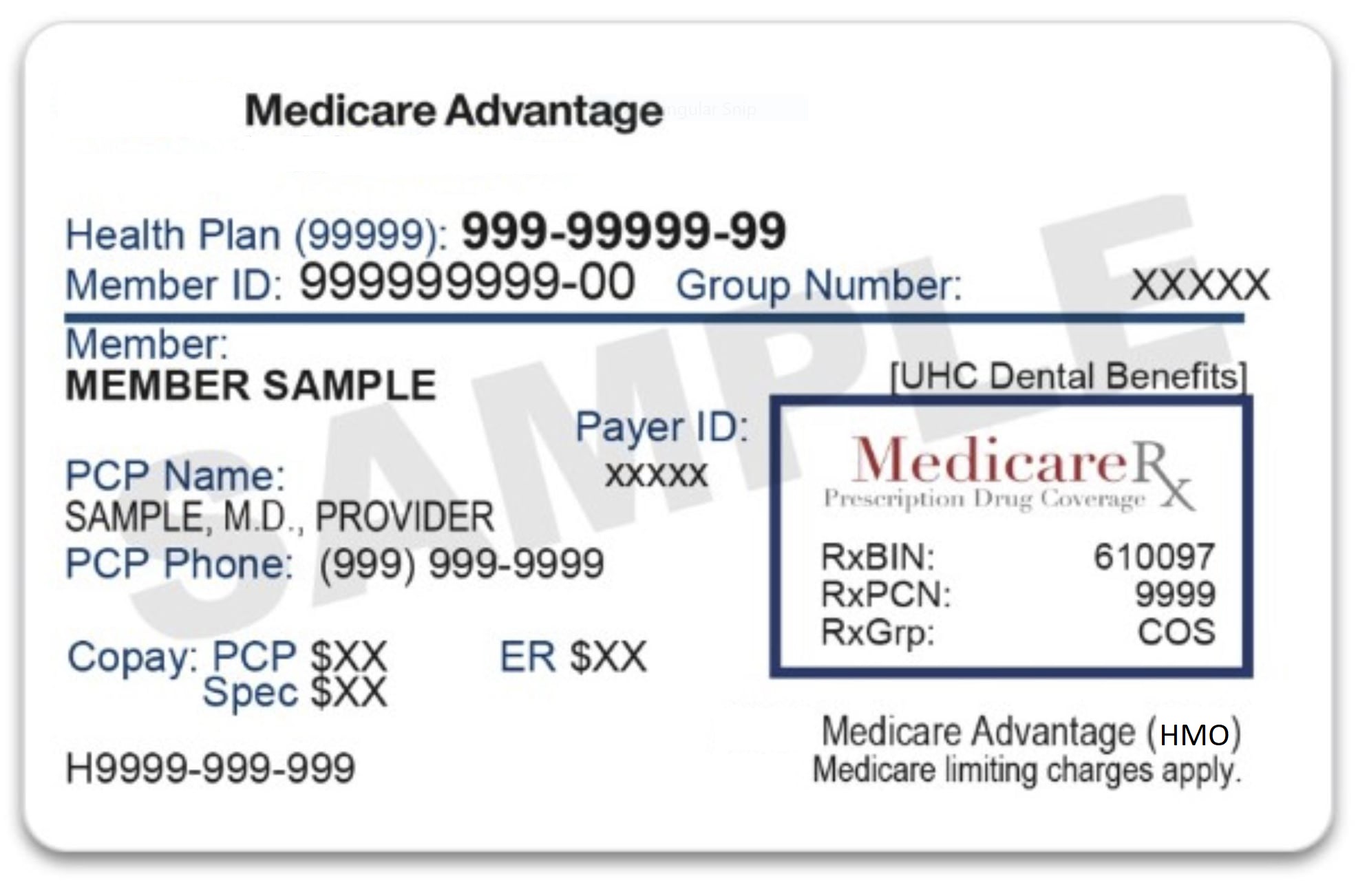
All Florida Special Needs Plans must provide Medicare Prescription drug coverage (Part D).
Do I need to choose a primary care doctor?
Some SNPs in Florida require primary care doctors and some don't. Check with the plan to see if you need to choose a primary care doctor.