Preferred Provider Organization (PPO) 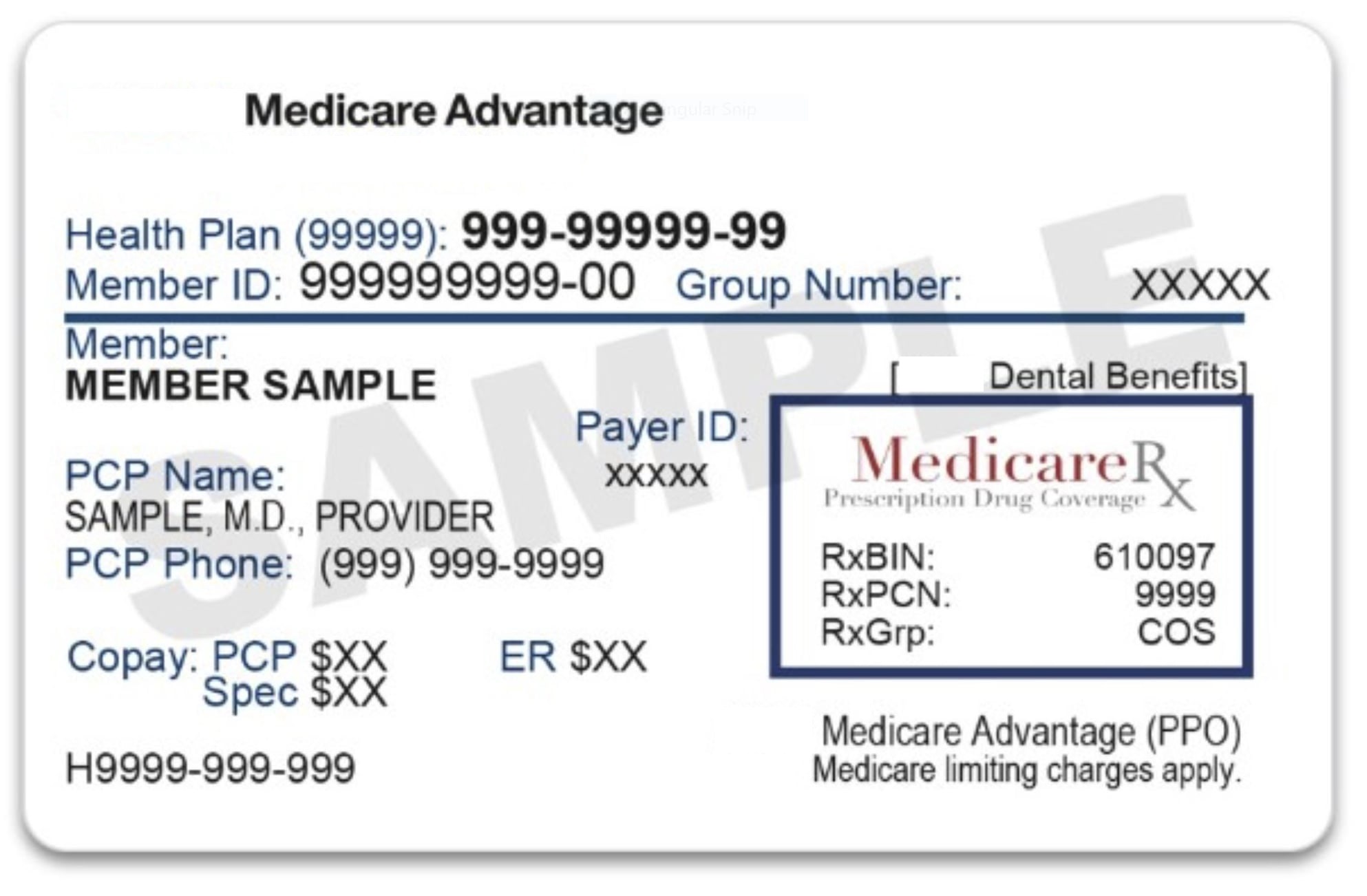
How Medicare PPO Network Plans Work
PPO stands for Preferred Provider Organization, which is another type of managed healthcare system. Medicare recipients In a Florida PPO, pay a monthly premium and in exchange, they have access to a network of healthcare providers who have agreed to provide services at a discounted rate. Unlike an HMO, Medicare patients in a Florida PPO are not required to choose a primary care physician and can see any provider within the network without a referral. Patients can also see providers outside of the network, but they may be subject to higher out-of-pocket costs that is if the provider agrees to treat you and hasn’t opted out of Medicare (for Medicare Part A and Part B items and services). PPOs offer more flexibility than HMOs, but they can also be more expensive. You’re always covered for emergency and urgent care.
Can you get your health care from any doctor, other health care provider, or hospital?
In most cases, you can get your health care from any doctor, other health care provider, or hospital in PPO Plans. Each plan gives you flexibility to go to doctors, specialists, or hospitals that aren't on the plan's list, but it will usually cost more.
Are prescription drugs covered?
In most cases, prescription drugs are covered in PPO Plans. Ask the plan. If you want Medicare drug coverage, you must join a PPO Plan that offers prescription drug coverage. Remember, if you join a PPO Plan that doesn't offer prescription drug coverage, you can't join a Medicare drug plan (Part D).
Do you need to choose a primary care doctor?
Medicare Advantage recipients in Florida don't need to choose a primary care doctor in PPO Plans.
Do you have to get a referral to see a specialist?
In most cases, no. But if you use plan specialists (in-network), your costs for covered services will usually be lower than if you use non-plan specialists (out-of-network).
What else do you need to know about this type of plan?
- Because certain providers are “preferred,” you can save money by using them.
- Check with the plan for more information.
Networks consist of : The facilities,
providers, and suppliers your health insurer or plan has
contracted with to provide health care services.


