Medicaid
Medicaid is a joint federal and state program that provides healthcare coverage to low-income individuals and families, as well as to people with certain disabilities. The program is administered by individual states, but it is funded by both the federal government and the states.
Qualifying for Medicaid Assistance
Medicaid covers a wide range of healthcare services, including doctor visits, hospital care, prescription drugs, and nursing home care. Eligibility for Medicaid is based on income and other factors, such as age, disability, and pregnancy. Each state has its own rules and eligibility requirements, but all states must cover certain mandatory benefits, such as inpatient and outpatient hospital care, physician services, and laboratory and x-ray services.
Medicaid is an important safety net for millions of Americans who might otherwise go without healthcare. It is also a significant source of funding for healthcare providers, particularly safety-net hospitals that serve a large number of Medicaid patients.
The income level required to qualify for Medicaid varies depending on the state you live in, as each state has its own rules and eligibility criteria. However, the Affordable Care Act (ACA) expanded Medicaid eligibility to all individuals with incomes up to 138% of the federal poverty level (FPL) in states that chose to implement the expansion. As of April 2023, 39 states plus the District of Columbia have implemented the Medicaid expansion.
For the year 2023, the federal poverty level guidelines set by the U.S. Department of Health and Human Services (HHS) are $13,590 for an individual and $27,950 for a family of four. Therefore, in states that have not expanded Medicaid, the income threshold for Medicaid eligibility is typically below 138% of the federal poverty level.
It's important to note that Medicaid eligibility is not just based on income, but also takes into account other factors such as age, disability, pregnancy, and citizenship status.
What Costs Medicaid helps pay for
If you have Medicare and qualify for full Medicaid coverage:- Your state will pay your Medicare Part B (Medical Insurance) monthly premiums.
- Depending on the level of Medicaid you qualify for, the state of Florida might pay for:
- Your share of Medicare costs, such as deductibles, coinsurance, and co-payments
- Part A (Hospital Insurance) premiums, if you have to pay a premium for that coverage.
- You'll automatically get Low Income Subsidy (LIS) Extra Help with your Part D drug costs.
- Medicaid may pay for other prescription drugs and services that Medicare does not cover.
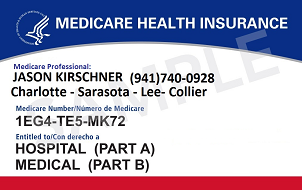
Dual Eligible Beneficiaries who qualified both Medicare & Medicaid
Dual eligible Medicare refers to individuals who are eligible for both Medicare and Medicaid. Medicare is a federal health insurance program that covers individuals aged 65 and older, as well as certain younger individuals with disabilities or certain medical conditions. Medicaid, on the other hand, is a joint federal and state program that provides health coverage for low-income individuals and families.
Dual eligible Medicare beneficiaries are typically individuals with low incomes and limited resources, who qualify for both Medicare and Medicaid. These individuals receive coverage for their medical care from both programs, with Medicare covering most of their medical expenses and Medicaid filling in coverage gaps, such as co-payments and deductibles.
You can still pick how you want to get your Medicare coverage: Original Medicare or a Dual Special Needs Plan through Medicare Advantage (Part C)
Some of the benefits available to dual eligible Medicare beneficiaries include hospital stays, physician visits, prescription drugs, and long-term care. The specific benefits available to each beneficiary may vary depending on their individual circumstances and the state in which they live.
Medicare Savings Programs
Medicare Savings Programs (MSPs) are state run health programs that help low-income Medicare beneficiaries pay for their Medicare premiums and out-of-pocket costs. There are four types of MSPs:
- Qualified Medicare Beneficiary (QMB) Program: This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance, and copayments for those who meet certain income and asset limits.
- Specified Low-Income Medicare Beneficiary (SLMB) Program: This program helps pay for Medicare Part B premiums for those who meet certain income and asset limits.
- Qualifying Individual (QI) Program: This program helps pay for Medicare Part B premiums for those who meet certain income and asset limits. However, funding for this program is limited, so not all eligible individuals may receive assistance.
- Qualified Disabled and Working Individuals (QDWI) Program: This program helps pay for Medicare Part A premiums for certain disabled individuals who are working and meet certain income and asset limits.
To qualify for an MSP, individuals must meet certain income and asset limits set by their state. The eligibility criteria may vary from state to state, so it is important to check with the state's Medicaid agency to determine the specific requirements