Health Maintenance Organization (HMO) 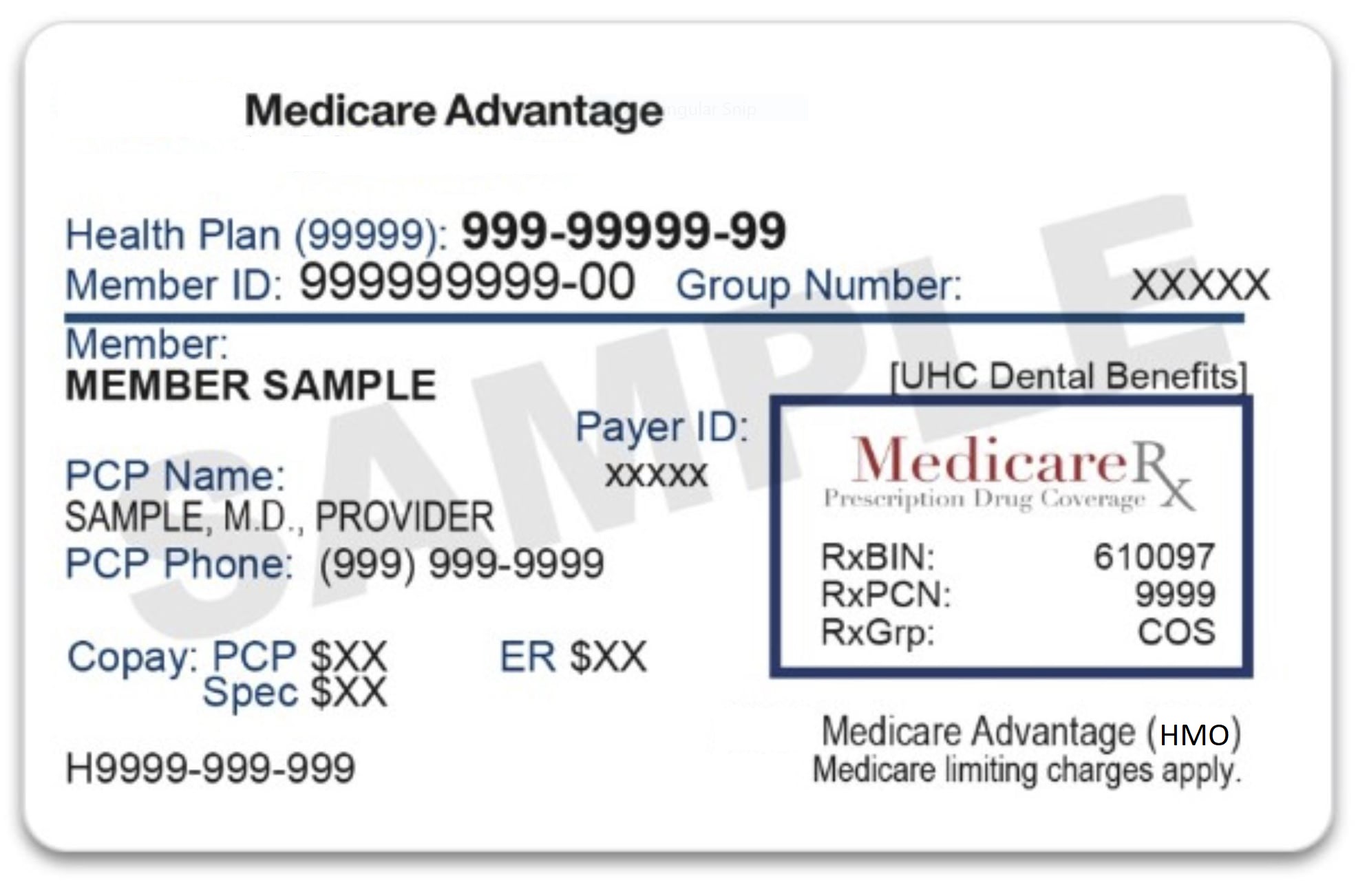
HMO stands for Health Maintenance Organization, which is a type of managed healthcare system in Florida. In an HMO, individuals pay a monthly premium and in exchange, they receive access to a network of healthcare providers who offer services at a reduced cost. Patients typically choose a primary care physician from within the HMO network, who serves as their main point of contact for all healthcare needs. The primary care physician may refer patients to specialists within the network as needed. HMOs are known for their emphasis on preventative care and cost containment, but they can also limit a patient's choice of healthcare providers.
In HMO Plans, beneficiaries generally must get their care and services from doctors, other health care providers, and hospitals in the Florida plans network, except:
- Emergency care
- Out-of-area urgent care
- Temporary out-of-area dialysis
HMO Point-of-Service (HMO-POS) plans are HMO plans in Florida that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when the plan requires it.
Are prescription drugs covered in Health Maintenance Organization (HMO) Plans?
In most cases, prescription drugs are covered in HMO Plans. Ask the plan. If you want Medicare drug coverage (Part D), Florida seniors must join an HMO Plan that offers prescription drug coverage. If you join an HMO plan without drug coverage, you can’t join a separate Medicare drug plan.
Do I need to choose a primary care doctor in Health Maintenance Organization (HMO) Plans?
In most cases, yes, you need to choose a primary care doctor in HMO Plans.
Do I have to get a referral to see a specialist in Health Maintenance Organization (HMO) Plans?
In most cases you have to get a referral to see a specialist in HMO Plans. Certain services, like yearly screening mammograms, don't require a referral.
What else do Medicare enrollees 65 in Florida need to know about this type of Medicare Advantage plan?
- If your doctor or other health care provider leaves the plan, your plan will notify you. You can choose another doctor in the plan.
- If you get health care outside the plan's network , you may have to pay the full cost.
- It's important that you follow the plan's rules, like getting prior approval for a certain service when needed.
Networks consist of : The facilities,
providers, and suppliers your health insurer or plan has
contracted with to provide health care services.